Abstract
Cardiovascular disease complicates 1–4% of pregnancies — with a higher prevalence when including hypertensive disorders — and is the leading cause of maternal death. In women with known cardiovascular pathology, such as congenital heart disease, timely counselling is possible and the outcome is fairly good. By contrast, maternal mortality is high in women with acquired heart disease that presents during pregnancy (such as acute coronary syndrome or aortic dissection). Worryingly, the prevalence of acquired cardiovascular disease during pregnancy is rising as older maternal age, obesity, diabetes mellitus and hypertension become more common in the pregnant population. Management of cardiovascular disease in pregnancy is challenging owing to the unique maternal physiology, characterized by profound changes to multiple organ systems. The presence of the fetus compounds the situation because both the cardiometabolic disease and its management might adversely affect the fetus. Equally, avoiding essential treatment because of potential fetal harm risks a poor outcome for both mother and child. In this Review, we examine how the physiological adaptations during pregnancy can provoke cardiometabolic complications or exacerbate existing cardiometabolic disease and, conversely, how cardiometabolic disease can compromise the adaptations to pregnancy and their intended purpose: the development and growth of the fetus.
Key points
-
Cardiovascular disease complicates 1–4% of pregnancies — with a higher prevalence when hypertensive disorders are included — and accounts for 16% of maternal mortality, making cardiovascular diseases the leading cause of death in pregnant women in developed countries.
-
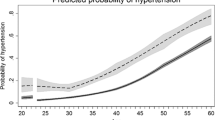
Advanced maternal age, obesity, hypertension, smoking and diabetes mellitus are all major cardiovascular risk factors that are increasingly prevalent in the pregnant population.
-
Profound haemodynamic changes, such as a 50% increase in cardiac output, place a burden on the maternal cardiovascular system during pregnancy and can provoke new-onset or an exacerbation of existing cardiovascular disease.
-
When prescribing medication, the altered pharmacokinetics during pregnancy should be considered in addition to fetal safety, and regular serum measurements can be beneficial because drug concentrations can change.
-
During pregnancy, a high index of suspicion and a low threshold for investigation of cardiometabolic diseases is warranted.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Regitz-Zagrosek, V. et al. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Kardiol. Pol. 77, 245–326 (2019).
Duley, L. The global impact of pre-eclampsia and eclampsia. Semin. Perinatol. 33, 130–137 (2009).
Sliwa, K. & Bohm, M. Incidence and prevalence of pregnancy-related heart disease. Cardiovasc. Res. 101, 554–560 (2014).
Knight, M. N. M., Tuffnell, D., Shakespeare, J., Kenyon, S. & Kurinczuk, J. J. Saving lives, improving mothers’ care — lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2013–2015. MBRRACE-UK https://www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/MBRRACE-UK%20Maternal%20Report%202017%20-%20Web.pdf (2017).
Cantwell, R. et al. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 2006–2008. The eighth report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG 118 (Suppl. 1), 1–203 (2011).
Creanga, A. A., Syverson, C., Seed, K. & Callaghan, W. M. Pregnancy-related mortality in the United States, 2011–2013. Obstet. Gynecol. 130, 366–373 (2017).
Martin, J. A., Hamilton, B. E., Osterman, M. J. K. & Driscoll, A. K. Births: final data for 2018. Natl Vital. Stat. Rep. 68, 47 (2019).
Stephen, E. H., Chandra, A. & King, R. B. Supply of and demand for assisted reproductive technologies in the United States: clinic- and population-based data, 1995–2010. Fertil. Steril. 105, 451–458 (2016).
Laopaiboon, M. et al. Advanced maternal age and pregnancy outcomes: a multicountry assessment. BJOG 121 (Suppl. 1), 49–56 (2014).
Kuklina, E. V., Ayala, C. & Callaghan, W. M. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet. Gynecol. 113, 1299–1306 (2009).
Albrecht, S. S. et al. Diabetes trends among delivery hospitalizations in the U.S., 1994–2004. Diabetes Care 33, 768–773 (2010).
Hinkle, S. N. et al. Prepregnancy obesity trends among low-income women, United States, 1999–2008. Matern. Child Health J. 16, 1339–1348 (2012).
Fisher, S. C., Kim, S. Y., Sharma, A. J., Rochat, R. & Morrow, B. Is obesity still increasing among pregnant women? Prepregnancy obesity trends in 20 states, 2003–2009. Prev. Med. 56, 372–378 (2013).
Creamer, M. R. et al. Tobacco product use and cessation indicators among adults — United States, 2018. MMWR Morb. Mortal. Wkly. Rep. 68, 1013–1019 (2019).
Jamal, A. et al. Current cigarette smoking among adults — United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 67, 53–59 (2018).
Chevalier, N. et al. Materno-fetal cardiovascular complications in Turner syndrome after oocyte donation: insufficient prepregnancy screening and pregnancy follow-up are associated with poor outcome. J. Clin. Endocrinol. Metab. 96, E260–E267 (2011).
Hagman, A. et al. Obstetric and neonatal outcome after oocyte donation in 106 women with Turner syndrome: a Nordic cohort study. Hum. Reprod. 28, 1598–1609 (2013).
Roos-Hesselink, J. et al. Pregnancy outcomes in women with cardiovascular disease: evolving trends over 10 years in the ESC registry of pregnancy and cardiac disease (ROPAC). Eur. Heart J. 40, 3848–3855 (2019).
Duvekot, J. J., Cheriex, E. C., Pieters, F. A., Menheere, P. P. & Peeters, L. H. Early pregnancy changes in hemodynamics and volume homeostasis are consecutive adjustments triggered by a primary fall in systemic vascular tone. Am. J. Obstet. Gynecol. 169, 1382–1392 (1993).
Duvekot, J. J. & Peeters, L. L. Maternal cardiovascular hemodynamic adaptation to pregnancy. Obstet. Gynecol. Surv. 49, S1–S14 (1994).
Capeless, E. L. & Clapp, J. F. Cardiovascular changes in early phase of pregnancy. Am. J. Obstet. Gynecol. 161, 1449–1453 (1989).
Ochsenbein-Kolble, N. et al. Cross sectional study of automated blood pressure measurements throughout pregnancy. BJOG 111, 319–325 (2004).
Lopes van Balen, V. A. et al. Maternal kidney function during pregnancy: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 54, 297–307 (2019).
de Haas, S., Ghossein-Doha, C., van Kuijk, S. M., van Drongelen, J. & Spaanderman, M. E. Physiological adaptation of maternal plasma volume during pregnancy: a systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 49, 177–187 (2017).
McGuane, J. T. et al. Role of relaxin in maternal systemic and renal vascular adaptations during gestation. Ann. N. Y. Acad. Sci. 1160, 304–312 (2009).
Odutayo, A. & Hladunewich, M. Obstetric nephrology: renal hemodynamic and metabolic physiology in normal pregnancy. Clin. J. Am. Soc. Nephrol. 7, 2073–2080 (2012).
Whittaker, P. G., Macphail, S. & Lind, T. Serial hematologic changes and pregnancy outcome. Obstet. Gynecol. 88, 33–39 (1996).
Meah, V. L., Cockcroft, J. R., Backx, K., Shave, R. & Stohr, E. J. Cardiac output and related haemodynamics during pregnancy: a series of meta-analyses. Heart 102, 518–526 (2016).
Hunter, S. & Robson, S. C. Adaptation of the maternal heart in pregnancy. Br. Heart J. 68, 540–543 (1992).
Robson, S. C., Hunter, S., Boys, R. J. & Dunlop, W. Serial study of factors influencing changes in cardiac output during human pregnancy. Am. J. Physiol. 256, H1060–H1065 (1989).
De Haas, S. et al. Cardiac remodeling in normotensive pregnancy and in pregnancy complicated by hypertension: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 50, 683–696 (2017).
Robson, S. C., Dunlop, W., Boys, R. J. & Hunter, S. Cardiac output during labour. Br. Med. J. 295, 1169–1172 (1987).
Ruys, T. P. et al. Heart failure in pregnant women with cardiac disease: data from the ROPAC. Heart 100, 231–238 (2014).
Shiozaki, A., Matsuda, Y., Satoh, S. & Saito, S. Comparison of risk factors for gestational hypertension and preeclampsia in Japanese singleton pregnancies. J. Obstet. Gynaecol. Res. 39, 492–499 (2013).
Hellgren, M. & Blomback, M. Studies on blood coagulation and fibrinolysis in pregnancy, during delivery and in the puerperium. I. Normal condition. Gynecol. Obstet. Invest. 12, 141–154 (1981).
Rodger, M., Sheppard, D., Gandara, E. & Tinmouth, A. Haematological problems in obstetrics. Best. Pract. Res. Clin. Obstet. Gynaecol. 29, 671–684 (2015).
Peck, T. M. & Arias, F. Hematologic changes associated with pregnancy. Clin. Obstet. Gynecol. 22, 785–798 (1979).
Kowalska-Kanka, A., Maciejewski, T. & Niemiec, K. T. The role and regulation of secretion of erythropoietin in pregnancy. Med. Wieku Rozwoj 17, 270–275 (2013).
Angueira, A. R. et al. New insights into gestational glucose metabolism: lessons learned from 21st century approaches. Diabetes 64, 327–334 (2015).
Newbern, D. & Freemark, M. Placental hormones and the control of maternal metabolism and fetal growth. Curr. Opin. Endocrinol. Diabetes Obes. 18, 409–416 (2011).
Marcinkevage, J. A. & Narayan, K. M. Gestational diabetes mellitus: taking it to heart. Prim. Care Diabetes 5, 81–88 (2011).
Rees, G. B., Broughton Pipkin, F., Symonds, E. M. & Patrick, J. M. A longitudinal study of respiratory changes in normal human pregnancy with cross-sectional data on subjects with pregnancy-induced hypertension. Am. J. Obstet. Gynecol. 162, 826–830 (1990).
Hegewald, M. J. & Crapo, R. O. Respiratory physiology in pregnancy. Clin. Chest Med. 32, 1–13 (2011).
Gee, J. B., Packer, B. S., Millen, J. E. & Robin, E. D. Pulmonary mechanics during pregnancy. J. Clin. Invest. 46, 945–952 (1967).
Norregaard, O., Schultz, P., Ostergaard, A. & Dahl, R. Lung function and postural changes during pregnancy. Respir. Med. 83, 467–470 (1989).
Roy, C. et al. Fast imaging MR assessment of ureterohydronephrosis during pregnancy. Magn. Reson. Imaging 13, 767–772 (1995).
Faundes, A., Bricola-Filho, M. & Pinto e Silva, J. L. Dilatation of the urinary tract during pregnancy: proposal of a curve of maximal caliceal diameter by gestational age. Am. J. Obstet. Gynecol. 178, 1082–1086 (1998).
Erman, A. et al. Enhanced urinary albumin excretion after 35 weeks of gestation and during labour in normal pregnancy. Scand. J. Clin. Lab. Invest. 52, 409–413 (1992).
Steegers, E. A., von Dadelszen, P., Duvekot, J. J. & Pijnenborg, R. Pre-eclampsia. Lancet 376, 631–644 (2010).
World Health Organization. WHO Recommendations for Prevention and Treatment of Pre-Eclampsia and Eclampsia (World Health Organization, 2011).
Creanga, A. A. Maternal mortality in the United States: a review of contemporary data and their limitations. Clin. Obstet. Gynecol. 61, 296–306 (2018).
Khan, K. S., Wojdyla, D., Say, L., Gulmezoglu, A. M. & Van Look, P. F. WHO analysis of causes of maternal death: a systematic review. Lancet 367, 1066–1074 (2006).
Ananth, C. V., Keyes, K. M. & Wapner, R. J. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ 347, f6564 (2013).
Say, L. et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob. Health 2, e323–e333 (2014).
Khong, T. Y., De Wolf, F., Robertson, W. B. & Brosens, I. Inadequate maternal vascular response to placentation in pregnancies complicated by pre-eclampsia and by small-for-gestational age infants. Br. J. Obstet. Gynaecol. 93, 1049–1059 (1986).
Hylenius, S., Andersen, A. M., Melbye, M. & Hviid, T. V. Association between HLA-G genotype and risk of pre-eclampsia: a case-control study using family triads. Mol. Hum. Reprod. 10, 237–246 (2004).
Vanderlelie, J. et al. Increased biological oxidation and reduced anti-oxidant enzyme activity in pre-eclamptic placentae. Placenta 26, 53–58 (2005).
Hung, T. H., Charnock-Jones, D. S., Skepper, J. N. & Burton, G. J. Secretion of tumor necrosis factor-alpha from human placental tissues induced by hypoxia-reoxygenation causes endothelial cell activation in vitro: a potential mediator of the inflammatory response in preeclampsia. Am. J. Pathol. 164, 1049–1061 (2004).
Burton, G. J., Yung, H. W., Cindrova-Davies, T. & Charnock-Jones, D. S. Placental endoplasmic reticulum stress and oxidative stress in the pathophysiology of unexplained intrauterine growth restriction and early onset preeclampsia. Placenta 30 (Suppl. A), S43–S48 (2009).
Milne, F. et al. Assessing the onset of pre-eclampsia in the hospital day unit: summary of the pre-eclampsia guideline (PRECOG II). BMJ 339, b3129 (2009).
The American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 202: gestational hypertension and preeclampsia. Obstet. Gynecol. 133, e1–e25 (2019).
Valensise, H., Vasapollo, B., Gagliardi, G. & Novelli, G. P. Early and late preeclampsia: two different maternal hemodynamic states in the latent phase of the disease. Hypertension 52, 873–880 (2008).
Brown, M. A. et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 72, 24–43 (2018).
Altman, D. et al. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie trial: a randomised placebo-controlled trial. Lancet 359, 1877–1890 (2002).
Hoffman, M. K. et al. Low-dose aspirin for the prevention of preterm delivery in nulliparous women with a singleton pregnancy (ASPIRIN): a randomised, double-blind, placebo-controlled trial. Lancet 395, 285–293 (2020).
Roberge, S., Bujold, E. & Nicolaides, K. H. Aspirin for the prevention of preterm and term preeclampsia: systematic review and metaanalysis. Am. J. Obstet. Gynecol. 218, 287–293.e1 (2018).
Rolnik, D. L. et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N. Engl. J. Med. 377, 613–622 (2017).
LeFevre, N. & Krumm, E. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Am. Fam. Physician 100, 403–405 (2019).
Koopmans, C. M. et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet 374, 979–988 (2009).
Redman, E. K., Hauspurg, A., Hubel, C. A., Roberts, J. M. & Jeyabalan, A. Clinical course, associated factors, and blood pressure profile of delayed-onset postpartum preeclampsia. Obstet. Gynecol. 134, 995–1001 (2019).
Tooher, J. et al. All hypertensive disorders of pregnancy increase the risk of future cardiovascular disease. Hypertension 70, 798–803 (2017).
Zhu, Y. & Zhang, C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr. Diab Rep. 16, 7 (2016).
Group, H. S. C. R. et al. Hyperglycemia and adverse pregnancy outcomes. N. Engl. J. Med. 358, 1991–2002 (2008).
Fadl, H. E., Ostlund, I. K., Magnuson, A. F. & Hanson, U. S. Maternal and neonatal outcomes and time trends of gestational diabetes mellitus in Sweden from 1991 to 2003. Diabet. Med. 27, 436–441 (2010).
Petitt, D. J., Bennett, P. H., Knowler, W. C., Baird, H. R. & Aleck, K. A. Gestational diabetes mellitus and impaired glucose tolerance during pregnancy. Long-term effects on obesity and glucose tolerance in the offspring. Diabetes 34 (Suppl. 2), 119–122 (1985).
Rizzo, T. A., Metzger, B. E., Dooley, S. L. & Cho, N. H. Early malnutrition and child neurobehavioral development: insights from the study of children of diabetic mothers. Child Dev. 68, 26–38 (1997).
Bellamy, L., Casas, J. P., Hingorani, A. D. & Williams, D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373, 1773–1779 (2009).
Camprubi Robles, M. et al. Maternal diabetes and cognitive performance in the offspring: a systematic review and meta-analysis. PLoS One 10, e0142583 (2015).
Zhang, C., Rawal, S. & Chong, Y. S. Risk factors for gestational diabetes: is prevention possible? Diabetologia 59, 1385–1390 (2016).
Dooley, S. L., Metzger, B. E., Cho, N. & Liu, K. The influence of demographic and phenotypic heterogeneity on the prevalence of gestational diabetes mellitus. Int. J. Gynaecol. Obstet. 35, 13–18 (1991).
Catalano, P. M. Trying to understand gestational diabetes. Diabet. Med. 31, 273–281 (2014).
Li, Y. et al. Maternal age and the risk of gestational diabetes mellitus: a systematic review and meta-analysis of over 120 million participants. Diabetes Res. Clin. Pract. 162, 108044 (2020).
American Diabetes Association. 14. Management of diabetes in pregnancy: standards of medical care in diabetes-2020. Diabetes Care 43, S183–S192 (2020).
National Collaborating Centre for Women’s and Children’s Health. Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period (NICE, 2015).
Agarwal, M. M., Dhatt, G. S. & Punnose, J. Gestational diabetes: an alternative, patient-friendly approach for using the diagnostic 100-g OGTT in high-risk populations. Arch. Gynecol. Obstet. 273, 325–330 (2006).
Crowther, C. A. et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N. Engl. J. Med. 352, 2477–2486 (2005).
Lauenborg, J. et al. The prevalence of the metabolic syndrome in a Danish population of women with previous gestational diabetes mellitus is three-fold higher than in the general population. J. Clin. Endocrinol. Metab. 90, 4004–4010 (2005).
James, A. H., Jamison, M. G., Brancazio, L. R. & Myers, E. R. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am. J. Obstet. Gynecol. 194, 1311–1315 (2006).
Jacobsen, A. F., Skjeldestad, F. E. & Sandset, P. M. Incidence and risk patterns of venous thromboembolism in pregnancy and puerperium — a register-based case-control study. Am. J. Obstet. Gynecol. 198, 233 e1–7 (2008).
Heit, J. A. et al. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann. Intern. Med. 143, 697–706 (2005).
Macklon, N. S., Greer, I. A. & Bowman, A. W. An ultrasound study of gestational and postural changes in the deep venous system of the leg in pregnancy. Br. J. Obstet. Gynaecol. 104, 191–197 (1997).
Cantu-Brito, C. et al. Cerebrovascular complications during pregnancy and postpartum: clinical and prognosis observations in 240 Hispanic women. Eur. J. Neurol. 18, 819–825 (2011).
Rova, K., Passmark, H. & Lindqvist, P. G. Venous thromboembolism in relation to in vitro fertilization: an approach to determining the incidence and increase in risk in successful cycles. Fertil. Steril. 97, 95–100 (2012).
Rotzinger, D. C. et al. Pulmonary embolism during pregnancy: a 17-year single-center retrospective MDCT pulmonary angiography study. Eur. Radiol. 30, 1780–1789 (2020).
Bauersachs, R. M. et al. Risk stratification and heparin prophylaxis to prevent venous thromboembolism in pregnant women. Thromb. Haemost. 98, 1237–1245 (2007).
Romualdi, E. et al. Anticoagulant therapy for venous thromboembolism during pregnancy: a systematic review and a meta-analysis of the literature. J. Thromb. Haemost. 11, 270–281 (2013).
Bates, S. M. et al. VTE, thrombophilia, antithrombotic therapy, and pregnancy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141, e691S–e736S (2012).
James, A. H. et al. Acute myocardial infarction in pregnancy: a United States population-based study. Circulation 113, 1564–1571 (2006).
Elkayam, U. et al. Pregnancy-associated acute myocardial infarction: a review of contemporary experience in 150 cases between 2006 and 2011. Circulation 129, 1695–1702 (2014).
Wingrove, C. S., Garr, E., Godsland, I. F. & Stevenson, J. C. 17beta-oestradiol enhances release of matrix metalloproteinase-2 from human vascular smooth muscle cells. Biochim. Biophys. Acta 1406, 169–174 (1998).
Manalo-Estrella, P. & Barker, A. E. Histopathologic findings in human aortic media associated with pregnancy. Arch. Pathol. 83, 336–341 (1967).
Kaadan, M. I. et al. Prospective cardiovascular genetics evaluation in spontaneous coronary artery dissection. Circ. Genom. Precis. Med. 11, e001933 (2018).
Gornik, H. L. et al. First international consensus on the diagnosis and management of fibromuscular dysplasia. J. Hypertens. 37, 229–252 (2019).
Ismail, S., Wong, C., Rajan, P. & Vidovich, M. I. ST-elevation acute myocardial infarction in pregnancy: 2016 update. Clin. Cardiol. 40, 399–406 (2017).
Karalis, D. G., Hill, A. N., Clifton, S. & Wild, R. A. The risks of statin use in pregnancy: a systematic review. J. Clin. Lipidol. 10, 1081–1090 (2016).
Shotan, A., Widerhorn, J., Hurst, A. & Elkayam, U. Risks of angiotensin-converting enzyme inhibition during pregnancy: experimental and clinical evidence, potential mechanisms, and recommendations for use. Am. J. Med. 96, 451–456 (1994).
Costantine, M. M. et al. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am. J. Obstet. Gynecol. 214, 720.e1–720.e17 (2016).
Winterfeld, U. et al. Pregnancy outcome following maternal exposure to statins: a multicentre prospective study. BJOG 120, 463–471 (2013).
Ersboll, A. S. et al. Peripartum cardiomyopathy in Denmark: a retrospective, population-based study of incidence, management and outcome. Eur. J. Heart Fail. 19, 1712–1720 (2017).
Isezuo, S. A. & Abubakar, S. A. Epidemiologic profile of peripartum cardiomyopathy in a tertiary care hospital. Ethn. Dis. 17, 228–233 (2007).
Sliwa, K. et al. Clinical characteristics of patients from the worldwide registry on peripartum cardiomyopathy (PPCM): EURObservational research programme in conjunction with the Heart Failure Association of the European Society of Cardiology Study Group on PPCM. Eur. J. Heart Fail. 19, 1131–1141 (2017).
Kolte, D. et al. Temporal trends in incidence and outcomes of peripartum cardiomyopathy in the United States: a nationwide population-based study. J. Am. Heart Assoc. 3, e001056 (2014).
Baris, L., Cornette, J., Johnson, M. R., Sliwa, K. & Roos-Hesselink, J. W. Peripartum cardiomyopathy: disease or syndrome? Heart 105, 357–362 (2019).
Hilfiker-Kleiner, D. et al. A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell 128, 589–600 (2007).
Bauersachs, J. et al. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur. J. Heart Fail. 21, 827–843 (2019).
Sliwa, K. et al. Evaluation of bromocriptine in the treatment of acute severe peripartum cardiomyopathy: a proof-of-concept pilot study. Circulation 121, 1465–1473 (2010).
Hilfiker-Kleiner, D. et al. Bromocriptine for the treatment of peripartum cardiomyopathy: a multicentre randomized study. Eur. Heart J. 38, 2671–2679 (2017).
US National Library of Medicine. ClinicalTrials.gov. https://clinicaltrials.gov//ct2/show/NCT02590601 (2017).
The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). The 2015 ESC guidelines for the management of infective endocarditis. Eur. Heart J. 36, 3036–3037 (2015).
Yuan, S. M. Infective endocarditis during pregnancy. J. Coll. Physicians Surg. Pak. 25, 134–139 (2015).
Kebed, K. Y. et al. Pregnancy and postpartum infective endocarditis: a systematic review. Mayo Clin. Proc. 89, 1143–1152 (2014).
Campuzano, K., Roque, H., Bolnick, A., Leo, M. V. & Campbell, W. A. Bacterial endocarditis complicating pregnancy: case report and systematic review of the literature. Arch. Gynecol. Obstet. 268, 251–255 (2003).
Montoya, M. E., Karnath, B. M. & Ahmad, M. Endocarditis during pregnancy. South. Med. J. 96, 1156–1157 (2003).
Kourtis, A. P., Read, J. S. & Jamieson, D. J. Pregnancy and infection. N. Engl. J. Med. 370, 2211–2218 (2014).
Kuijpers, J. M. et al. Incidence, risk factors, and predictors of infective endocarditis in adult congenital heart disease: focus on the use of prosthetic material. Eur. Heart J. 38, 2048–2056 (2017).
Sawlani, N., Shroff, A. & Vidovich, M. I. Aortic dissection and mortality associated with pregnancy in the United States. J. Am. Coll. Cardiol. 65, 1600–1601 (2015).
Thalmann, M. et al. Acute type A aortic dissection and pregnancy: a population-based study. Eur. J. Cardiothorac. Surg. 39, e159–e163 (2011).
Immer, F. F. et al. Aortic dissection in pregnancy: analysis of risk factors and outcome. Ann. Thorac. Surg. 76, 309–314 (2003).
Hart, M. V., Morton, M. J., Hosenpud, J. D. & Metcalfe, J. Aortic function during normal human pregnancy. Am. J. Obstet. Gynecol. 154, 887–891 (1986).
Gutin, L. S., Merz, A. E., Bakalov, V. K., Gharib, A. M. & Bondy, C. A. Parity and aortic dimensions in healthy women. Int. J. Cardiol. 165, 383–384 (2013).
Wolinsky, H. Effects of estrogen and progestogen treatment on the response of the aorta of male rats to hypertension. Morphological and chemical studies. Circ. Res. 30, 341–349 (1972).
Kamel, H., Roman, M. J., Pitcher, A. & Devereux, R. B. Pregnancy and the risk of aortic dissection or rupture: a cohort-crossover analysis. Circulation 134, 527–533 (2016).
Yates, M. T. et al. Perioperative management and outcomes of aortic surgery during pregnancy. J. Thorac. Cardiovasc. Surg. 149, 607–610 (2015).
Suzuki, T. et al. Type-selective benefits of medications in treatment of acute aortic dissection (from the international registry of acute aortic dissection [IRAD]). Am. J. Cardiol. 109, 122–127 (2012).
Vaidya, V. R. et al. Burden of arrhythmia in pregnancy. Circulation 135, 619–621 (2017).
Shotan, A., Ostrzega, E., Mehra, A., Johnson, J. V. & Elkayam, U. Incidence of arrhythmias in normal pregnancy and relation to palpitations, dizziness, and syncope. Am. J. Cardiol. 79, 1061–1064 (1997).
Li, J. M., Nguyen, C., Joglar, J. A., Hamdan, M. H. & Page, R. L. Frequency and outcome of arrhythmias complicating admission during pregnancy: experience from a high-volume and ethnically-diverse obstetric service. Clin. Cardiol. 31, 538–541 (2008).
Ertekin, E. et al. Ventricular tachyarrhythmia during pregnancy in women with heart disease: data from the ROPAC, a registry from the European Society of Cardiology. Int. J. Cardiol. 220, 131–136 (2016).
Brodsky, M. et al. New-onset ventricular tachycardia during pregnancy. Am. Heart J. 123, 933–941 (1992).
Tateno, S. et al. Arrhythmia and conduction disturbances in patients with congenital heart disease during pregnancy: multicenter study. Circ. J. 67, 992–997 (2003).
Fitton, C. A. et al. In-utero exposure to antihypertensive medication and neonatal and child health outcomes: a systematic review. J. Hypertens. 35, 2123–2137 (2017).
Chow, T., Galvin, J. & McGovern, B. Antiarrhythmic drug therapy in pregnancy and lactation. Am. J. Cardiol. 82, 58I–62I (1998).
Kozluk, E. et al. Catheter ablation of cardiac arrhythmias in pregnancy without fluoroscopy: a case control retrospective study. Adv. Clin. Exp. Med. 26, 129–134 (2017).
Boule, S. et al. Pregnancy in women with an implantable cardioverter-defibrillator: is it safe? Europace 16, 1587–1594 (2014).
Mitchell, A. A. et al. Medication use during pregnancy, with particular focus on prescription drugs: 1976–2008. Am. J. Obstet. Gynecol. 205, 51.e1–8 (2011).
Baron, T. H., Ramirez, B. & Richter, J. E. Gastrointestinal motility disorders during pregnancy. Ann. Intern. Med. 118, 366–375 (1993).
Maher, J. E. et al. Albumin levels in pregnancy: a hypothesis — decreased levels of albumin are related to increased levels of alpha-fetoprotein. Early Hum. Dev. 34, 209–215 (1993).
Pariente, G. et al. Pregnancy-associated changes in pharmacokinetics: a systematic review. PLoS Med. 13, e1002160 (2016).
Lopes van Balen, V. A. et al. Maternal kidney function during pregnancy: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 54, 297–307 (2018).
Mishanina, E. et al. Use of labour induction and risk of cesarean delivery: a systematic review and meta-analysis. CMAJ 186, 665–673 (2014).
Ruys, T. P. et al. Is a planned caesarean section in women with cardiac disease beneficial? Heart 101, 530–536 (2015).
Ramsey, P. S., Hogg, B. B., Savage, K. G., Winkler, D. D. & Owen, J. Cardiovascular effects of intravaginal misoprostol in the mid trimester of pregnancy. Am. J. Obstet. Gynecol. 183, 1100–1102 (2000).
Svanstrom, M. C. et al. Signs of myocardial ischaemia after injection of oxytocin: a randomized double-blind comparison of oxytocin and methylergometrine during caesarean section. Br. J. Anaesth. 100, 683–689 (2008).
Cauldwell, M. et al. The management of the third stage of labour in women with heart disease. Heart 103, 945–951 (2017).
Karamermer, Y. & Roos-Hesselink, J. W. Pregnancy and adult congenital heart disease. Expert. Rev. Cardiovasc. Ther. 5, 859–869 (2007).
Wu, P. et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 10, e003497 (2017).
Bellamy, L., Casas, J. P., Hingorani, A. D. & Williams, D. J. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 335, 974 (2007).
Wu, P. et al. Pre-eclampsia is associated with a twofold increase in diabetes: a systematic review and meta-analysis. Diabetologia 59, 2518–2526 (2016).
Basit, S., Wohlfahrt, J. & Boyd, H. A. Pre-eclampsia and risk of dementia later in life: nationwide cohort study. BMJ 363, k4109 (2018).
Covella, B. et al. A systematic review and meta-analysis indicates long-term risk of chronic and end-stage kidney disease after preeclampsia. Kidney Int. 96, 711–727 (2019).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks R. Cífková, P. Presbitero and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ramlakhan, K.P., Johnson, M.R. & Roos-Hesselink, J.W. Pregnancy and cardiovascular disease. Nat Rev Cardiol 17, 718–731 (2020). https://doi.org/10.1038/s41569-020-0390-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-020-0390-z
This article is cited by
-
Ferritin and iron supplements in gestational diabetes mellitus: less or more?
European Journal of Nutrition (2024)
-
Prevalence and determinants of maternal near miss in Ethiopia: a systematic review and meta-analysis, 2015–2023
BMC Women's Health (2023)
-
Preeclampsia-associated lncRNA FEZF1-AS1 regulates cell proliferation and apoptosis in placental trophoblast cells through the ELAVL1/NOC2L axis
Cell Division (2023)
-
Effect of endometrial thickness on obstetric and neonatal outcomes in assisted reproduction: a systematic review and meta-analysis
Reproductive Biology and Endocrinology (2023)
-
Maternal cardiovascular disorders before and during pregnancy and offspring cardiovascular risk across the life course
Nature Reviews Cardiology (2023)