Abstract
Purpose
The purpose of this systematic review is to describe the complications and downsides of robotic systems in total knee arthroplasty (TKA).
Methods
A comprehensive search according to the PRISMA guidelines was performed across PubMed, MEDLINE, Cochrane Central Register of Controlled Trials, Scopus, and Google Scholar from inception until December 2021. All articles of any study design directly reporting on complications and downsides of the robotic system in TKA were considered for inclusion. Risk of bias assessment was performed for all included studies using the Cochrane risk of bias and MINORS score.
Results
A total of 21 studies were included, consisting of 4 randomized controlled trials, 7 prospective studies and 10 retrospective studies. Complications of the robotic system were pin-hole fracture, pin-related infection, iatrogenic soft tissue and bony injury, and excessive blood loss. While, downsides were longer operative duration, higher intraoperative cost, learning curve and aborting a robotic TKA due to different reasons. Iatrogenic injuries were more common in the active robotic system and abortion of the robotic TKA was reported only with active robotic TKA.
Conclusion
Robotic TKA is associated with certain advantages and disadvantages. Therefore, surgeons need to be familiar with the system to use it effectively. Widespread adoption of the robotic system should always be evidence-based.
Level of evidence
IV.
Similar content being viewed by others
Introduction
Robotics was first introduced into orthopedics surgery in the 1980s to improve the accuracy in implant positioning, prosthesis alignment and to reduce the rate of complications compared to conventional manual techniques [28]. Robotic total knee arthroplasty enhances the surgeon’s preoperative planning capabilities and real-time intra-operative dynamic referencing to allow for continuous assessments of range of motion and ligamentous tensioning. The real-time intra-operative kinematic assessment allows the comparison between the osteoarthritic knee and the new prosthetic knee [22]. However, with a lack of long-term evidence comparing clinical and functional results with conventional TKA and associated with increased costs and longer operative time, the trust in robotic TKA is restricted [14]. We are now in a pivotal time when data are emerging on robotic technologies, which makes it prudent to objectively examine whether their potential benefits are being realized.
In orthopedic surgery, every procedure is associated with some complications. Hence, it is fundamental to systematically examine the complications to improve the understanding and decrease these complications. It is also necessary to systematically assess the complications of this new technology before it can be widely used. In a recent systematic review [35], pin-hole fractures were reported in robotic TKA. But, to authors’ knowledge, no systematic review is available that comprehensively described all reported complications and downsides of robotic TKA. Therefore, we performed a systematic review of studies that reported complications and downsides of robotic TKA. Based on the results of the study, surgeons can perform appropriate risk stratification, which can help to counsel patients and their families, when selecting patients for robotic TKA. The hypothesis was that robotic TKA is associated with certain complications and downsides.
Materials and methods
This systematic review followed Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) Guidelines for literature search and it was registered on the PROSPERO International prospective register of systematic reviews (ID CRD42022303970).
Search strategy
A literature review was performed using a strategy search designed to collect articles regarding complications and flaws of robotic TKA. Two independent authors (A.M., C.N.) conducted a comprehensive search across multiple databases (PubMed/MEDLINE, Cochrane Central Register of Controlled Trials, Scopus, and Google Scholar) and reviewed each article’s title and abstract for studies available until December 2021. Identified articles and their corresponding references were also reviewed according to selection criteria for additional eligible articles. The keywords used for initial screening were ((TKA) OR (TKR) OR (Total Knee Replacement) OR (Total Knee Arthroplasty)) AND ((Robot) OR (Robotic) OR (Robotic Surgical Procedure) OR (Robotic Arm Assisted)) AND ((Complication) OR (Disadvantage)). The full texts of the articles were obtained and evaluated when eligibility could not be assessed from the title and abstract. The eligibility of studies was independently assessed by these two authors and disagreements were resolved by consensus discussion between the authors, and a third author (C.F.) was consulted if the disagreement could not be resolved.
Inclusion and exclusion criteria
All articles of any study design directly reporting on complications and downsides of the robotic system in TKA were considered for inclusion. Intraoperative complications, such as pin-hole fracture, iatrogenic soft tissue and bony injury, excessive blood loss, longer operative duration, aborting a robotic TKA due to different reasons and postoperative issues, such as pin-related infection, longer hospital stays and post-TKA stiffness, were noted. Any other complications and downsides of this technology were also reported. Non-English studies, non-peer-reviewed studies, review articles, case reports, surgical techniques, conference abstracts, non-clinical studies as well as studies solely focused on robotic unicompartmental knee arthroplasty, computer-assisted total knee arthroplasty, or navigated total knee arthroplasty were excluded.
The Cochrane risk of bias (RoB1) tool for randomized controlled trials [12] and methodological index for non-randomized studies (MINORS) tool [33] for observational studies was used for the quality assessment of the included studies. Two authors (A.M, C.N.) independently performed the quality assessment for each article. A third author (C.F.) was consulted in case of disagreement.
Results
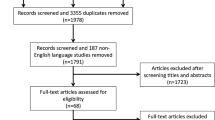
There were 530 potentially relevant studies identified in the initial comprehensive search across multi-databases and reference lists. Following the elimination of duplicate titles, abstracts were screened and pre-defined inclusion and exclusion criteria were applied. A large proportion of robotic-assisted surgeries was performed on unicompartmental knee arthroplasty (UKA) instead of TKA and hence, these studies were also excluded. A further 33 studies were excluded from analysis for various reasons after review of 54 full-text articles and one of the main reasons for exclusion was that data about complications were not available. Through discrete screenings, a total of 21 studies were included (Table 1), consisting of 4 randomized controlled trials, 7 prospective studies and 10 retrospective studies. A selection process flow diagram to identify included studies is presented in Fig. 1.
Methodological quality assessment
The Cochrane risk of bias (RoB1) tool was used for the quality assessment of 4 RCT studies. The MINORS criteria were used for the quality assessment of 17 observational studies and the average score was 15.9, ranging from 8 to 20. The quality assessment data are shown in Tables 2 and 3.
Pin-hole fracture [11, 29, 38, 39], pin-related infection [11, 15, 32, 36], iatrogenic injuries [11, 29, 36], more blood loss [11, 17] in the robotic TKA and stiffness after robotic TKA [20, 34] were the reported complications. Whereas, longer operative duration [7, 9, 11, 13, 17, 24, 26, 32, 34, 36, 38], longer hospital stays [27], higher intraoperative cost [2, 9], learning curve [15, 20, 22, 31, 32, 38], aborting a robotic TKA due to different reasons [8, 19, 32] were reported downsides. Iatrogenic injuries were more common in the active robotic system and abortion of the robotic TKA was reported only with active robotic TKA. The results of included studies are illustrated in Table 4.
Discussion
The most important finding of this systematic review was that robotic TKA is associated with longer operative time. Iatrogenic injuries were more common in the active robotic system and abortion of the robotic TKA was reported only with active robotic TKA.
Both, robotic and conventional systems have their advantages and disadvantages. Advantages of robotic TKA include accurate placement of prosthesis which results in fewer outliers in the component positions, superior implant alignment accuracy, precise bony cuts, and soft tissue balancing which are all considered a prerequisite for good functional outcome and endurance in TKA. A recent meta-analysis found improved short-term patient-reported outcomes (KSS and WOMAC) in the robotic group compared to the conventional TKA group [41]. However, these advantages of better clinical scores, patient satisfaction, and implant survivorship remain to be confirmed in long-term follow-up [18].
Three different robotic systems are available, based on the amount of autonomy delivered to both the surgeon and the robot, which include passive, active and semi-active. In a passive robotic system, the surgeon has continuous and direct control, while, an active robotic system is completely independent of the surgeon for performing a designated task. Therefore, active robotic systems are associated with increased chances of iatrogenic soft tissue injury. To ensure accuracy and safety against iatrogenic soft tissue or neurovascular injury, semi-active systems developed which provide tactile feedback to the surgeon, thus, helping define specific boundaries (i.e., for surgical resection or safety). The major goals of a semi-active system are to prevent gross intraoperative errors and reduce deviations from the surgical plan to ensure a safe procedure with well-aligned components. Although constant efforts have been made to improve the robotic system and decrease the associated complication, certain complications and downsides have been reported in the literature.
Femoral or tibial shaft fracture due to mechanical weakness caused by the pinholes is one of the most dreaded complications of the robotic TKA. In their study of 385 TKAs Beldame et al. [4] found the incidence of pin-site femoral fracture fractures to be 1.4%. They found a unique pattern of pin-site fracture where fractures occur an average of 12.6 weeks after arthroplasty, and before fracture episodes, patients experienced unusual pain for several days in the thigh. These fractures were associated with minor or indirect trauma and all of them were treated by intramedullary fixation. Yun et al. [39] and Baek et al. [3] recommended periarticular pin placement because the bone at this site is more robust to torsional and bending stresses than the diaphysis. Vermue et al. [38] advised for the smaller pins to prevent this complication. Preoperatively, all the patients should be informed about the potential risk of pin-hole fractures because it is not rare. Pin-site infection is another specific complication of tracker pin that may require antibiotics and dressing for an additional duration. However, the incidence of pin-site infection was reported to be low in general (0.47%) [11].
Iatrogenic soft tissue and bony injuries include patellar tendon rupture, dislocation of the patella, patellar fracture, and peroneal nerve injury [29]. Patellar tendon rupture was also seen in the study by Held et al. [11] and the patient underwent surgical repair. Although Kayani et al. [16] reported that Robotic TKA was associated with reduced bone and soft tissue injury compared to conventional TKA, other studies documented the opposite [11, 29, 36]. Iatrogenic injures were more common in active robotic system. Therefore, surgeons should be aware and try to avoid any iatrogenic injury while taking bone cuts.
In a recent study, Held et al. [11] found greater estimated blood loss in the robotic group which may be attributed to the prolonged operative time. In another long-term study by Kim et al. [17], the robotic group was associated with more blood loss and postoperative drainage volume. Bohl et al. [6] reported that longer surgical duration in hip and knee arthroplasty may require transfusion. However, it is important to recognize that robotic TKA does not require opening of the femoral canal which should theoretically result in less blood loss. Therefore, studies are needed with a large sample size to examine the difference in blood loss between these two groups.
Surgical robots are suggested to decrease post-TKA stiffness incidence by the accurate placement of a prosthesis and precise alignment but, this systematic review found studies that reported stiffness following robotic TKA. However, stiffness after TKA is multifactorial, in their recent systematic review, Zaffagini et al. [40] found modifiable and non-modifiable causes for post-TKA stiffness. Robots may help to correct the modifiable causes, such as prosthesis malalignment and overstuffing of joint but, other factors may not be corrected using robotic surgery.
This systematic review also identified some downsides of robotic systems compared to conventional instrumentation. The most consistent finding among different studies was longer intraoperative time with robotic systems. This longer duration is due to insertion and removal of pins in the femur and tibia, registration of the knee joint with the robotic system, and intraoperative planning. Longer surgical time is associated with a higher risk of infection which may result in devastating outcomes of TKA [25]. Pugely et al. [30] reported that after 120 min of surgical time the risk of infection increases to 1.8 times in joint arthroplasty. Two recent systematic reviews reported that the incidence of deep prosthetic joint infection was higher in robotic group at 1.6–1.7% compared to 0.44–1.0% in conventional TKA [21, 28]. Moreover, prolonged surgical duration is in part responsible for the higher intraoperative costs of robotic TKA. Other factors responsible for higher intraoperative costs were higher anesthesia costs, operation theater supplies, robotic maintenance costs, robotic-specific disposables costs, software requirements, and additional diagnostic imaging. On the other hand, some authors believe that robotic systems may improve TKA survivorship which would result in a decreased cost for future revision. However, to date, there is a lack of conclusive data on the relationship between the use of robotic systems and the longevity of TKA implants [1, 2, 10, 37]. Due to the additional time and expense associated with robotic systems in their long-term study, Kim 2019 et al. [17] did not recommend widespread use of robotic TKA.
There is conflicting evidence with respect to the length of hospital stay after robotic TKA. Most of the included studies reported shorter hospital stays in the robotic group, except for one study [27]. This was a nationwide database study from 2010 to 2017 which reported on significantly longer hospital stays following robotic TKA. Therefore, further research is needed for clarification of this matter.
Aborting a robotic TKA was another downside identified in this systematic review. Although all these studies used active robotic system. Regardless of the robotic system, reported abortion rates for robotic arthroplasty are between 1 and 12% [5]. Therefore, the surgeon should be aware of potential problems with the robotic system used, to avoid them upfront or to cope with them.
Another challenge with new technology is the learning curve. TKA robotics is associated with a learning curve that affects the comfort level of the surgical team. It has been shown that during this initial learning phase, the robotic system was associated with heightened levels of anxiety among the surgical team. This is an important consideration because stress and mental strain are correlated with diminished surgical performance, poor decision-making, and reduced technical skills [23]. The learning curve probably depends on the surgeon's previous experience and the general level of competence in robotics in surgery [20]. Therefore, surgeons starting with robotics TKA should foresee enough time to cope with this learning curve during initial cases.
This study has some key limitations. First, the heterogeneous approaches adopted in evaluating complications and downside of the robotic system did not allow a meta-analysis of the retrieved data. Second, the selection criteria, such as the exclusion of robotic unicompartmental knee arthroplasty, computer-assisted total knee arthroplasty or navigated total knee arthroplasty may have excluded relevant studies. Third, there are few studies on robotic TKAs and most of them are with small sample sizes with short-term follow-up. Future studies with large sample sizes and long-term follow-up will be needed to provide more conclusive findings in assessing the complications and downside of this system. Analysis of the national registry data will be a key finding to look out for the relevant complication associated with robotic TKA. Fourth, these studies used different robotic systems in different populations so there may be bias in the reporting of the complication.
The ultimate goal of the TKA is to create a stable, painless, long-lasting joint, which may be achieved by both conventional and robotic-assisted methods. The surgeon should be aware that despite the potential advantages of the robotic system, this new technology, may be associated with certain complications and downsides. This emerging technology is a tool, available to surgeons and they should decide which techniques will provide them and their patients with the optimum outcomes.
Conclusion
Robotic TKA is associated with certain advantages and disadvantages. Therefore, surgeons need to be familiar with the system to use it effectively. Widespread adoption of the robotic system should always be evidence-based.
References
Alesi D, Meena A, Fratini S, Rinaldi VG, Cammisa E, Lullini G, Vaccari V, Zaffagnini S, Marcheggiani Muccioli GM (2022) Total knee arthroplasty in valgus knee deformity: is it still a challenge in 2021? Musculoskelet Surg 106:1–8
Antonios JK, Korber S, Sivasundaram L, Mayfield C, Kang HP, Oakes DA, Heckmann ND (2019) Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: an analysis of patient and hospital factors. Arthroplasty Today 5:88–95
Baek J-H, Lee SC, Kim J-H, Ahn HS, Nam CH (2021) Distal femoral pin tracker placement prevents pin tract-induced fracture in robotic-assisted total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/s-0041-1735462
Beldame J, Boisrenoult P, Beaufils P (2010) Pin track induced fractures around computer-assisted TKA. Orthop Traumatol Surg Res 96:249–255
Bellemans J, Vandenneucker H, Vanlauwe J (2007) Robot-assisted total knee arthroplasty. Clin Orthop 464:111–116
Bohl DD, Ondeck NT, Darrith B, Hannon CP, Fillingham YA, Della Valle CJ (2018) Impact of operative time on adverse events following primary total joint arthroplasty. J Arthroplasty 33:2256-2262.e4
Bollars P, Boeckxstaens A, Mievis J, Kalaai S, Schotanus MGM, Janssen D (2020) Preliminary experience with an image-free handheld robot for total knee arthroplasty: 77 cases compared with a matched control group. Eur J Orthop Surg Traumatol 30:723–729
Chun YS, Kim KI, Cho YJ, Kim YH, Yoo MC, Rhyu KH (2011) Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty 26:621–625
Cotter EJ, Wang J, Illgen RL (2022) Comparative cost analysis of robotic-assisted and jig-based manual primary total knee arthroplasty. J Knee Surg 35:176–184
Fratini S, Meena A, Alesi D, Cammisa E, Zaffagnini S, Marcheggiani Muccioli GM (2022) Does implant design influence failure rate of lateral unicompartmental knee arthroplasty? A meta-analysis. J Arthroplasty 37(5):985–922
Held MB, Gazgalis A, Neuwirth AL, Shah RP, Cooper HJ, Geller JA (2021) Imageless robotic-assisted total knee arthroplasty leads to similar 24-month WOMAC scores as compared to conventional total knee arthroplasty: a retrospective cohort study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06599-4
Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928–d5928
Jeon S-W, Kim K-I, Song SJ (2019) Robot-assisted total knee arthroplasty does not improve long-term clinical and radiologic outcomes. J Arthroplasty 34:1656–1661
Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS (2019) Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev 4:611–617
Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS (2019) Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 27:1132–1141
Kayani B, Konan S, Pietrzak JRT, Haddad FS (2018) Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty 33:2496–2501
Kim Y-H, Yoon S-H, Park J-W (2020) Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized, controlled trial. Clin Orthop 478:266–275
Kort N, Stirling P, Pilot P, Müller JH (2021) Robot-assisted knee arthroplasty improves component positioning and alignment, but results are inconclusive on whether it improves clinical scores or reduces complications and revisions: a systematic overview of meta-analyses. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06472-4
Liow MHL, Goh GS-H, Wong MK, Chin PL, Tay DK-J, Yeo S-J (2017) Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 25:2942–2951
Mahure SA, Teo GM, Kissin YD, Stulberg BN, Kreuzer S, Long WJ (2021) Learning curve for active robotic total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06452-8
Mancino F, Cacciola G, Malahias M-A, De Filippis R, De Marco D, Di Matteo V, Gu A, Sculco PK, Maccauro G, De Martino I (2020) What are the benefits of robotic-assisted total knee arthroplasty over conventional manual total knee arthroplasty? A systematic review of comparative studies. Orthop Rev. https://doi.org/10.4081/or.2020.8657
Marchand RC, Sodhi N, Bhowmik-Stoker M, Scholl L, Condrey C, Khlopas A, Sultan AA, Newman JM, Mont MA (2019) Does the robotic arm and preoperative CT planning help with 3D intraoperative total knee arthroplasty planning? J Knee Surg 32:742–749
Marteau TM, Bekker H (1992) The development of a six-item short-form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br J Clin Psychol 31:301–306
Mitchell J, Wang J, Bukowski B, Greiner J, Wolford B, Oyer M, Illgen RL (2021) Relative clinical outcomes comparing manual and robotic-assisted total knee arthroplasty at minimum 1-year follow-up. HSS J Musculoskelet J Hosp Spec Surg 17:267–273
Naranje S, Lendway L, Mehle S, Gioe TJ (2015) Does operative time affect infection rate in primary total knee arthroplasty? Clin Orthop 473:64–69
Naziri Q, Cusson BC, Chaudhri M, Shah NV, Sastry A (2019) Making the transition from traditional to robotic-arm assisted TKA: what to expect? A single-surgeon comparative-analysis of the first-40 consecutive cases. J Orthop 16:364–368
Ofa SA, Ross BJ, Flick TR, Patel AH, Sherman WF (2020) Robotic total knee arthroplasty vs conventional total knee arthroplasty: a nationwide database study. Arthroplasty Today 6:1001-1008.e3
Onggo JR, Onggo JD, De Steiger R, Hau R (2020) Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: a meta-analysis and systematic review. Arch Orthop Trauma Surg 140:1533–1549
Park SE, Lee CT (2007) Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 22:1054–1059
Pugely AJ, Martin CT, Gao Y, Schweizer ML, Callaghan JJ (2015) The incidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplasty 30:47–50
Savov P, Tuecking L-R, Windhagen H, Ehmig J, Ettinger M (2021) Imageless robotic handpiece-assisted total knee arthroplasty: a learning curve analysis of surgical time and alignment accuracy. Arch Orthop Trauma Surg 141:2119–2128
Siebert W, Mai S, Kober R, Heeckt PF (2002) Technique and first clinical results of robot-assisted total knee replacement. Knee 9:173–180
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Smith AF, Eccles CJ, Bhimani SJ, Denehy KM, Bhimani RB, Smith LS, Malkani AL (2021) Improved patient satisfaction following robotic-assisted total knee arthroplasty. J Knee Surg 34:730–738
Smith TJ, Siddiqi A, Forte SA, Judice A, Sculco PK, Vigdorchik JM, Schwarzkopf R, Springer BD (2021) Periprosthetic fractures through tracking pin sites following computer navigated and robotic total and unicompartmental knee arthroplasty: a systematic review. JBJS Rev 9(e20):00091
Song E-K, Seon J-K, Yim J-H, Netravali NA, Bargar WL (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop 471:118–126
de Steiger RN, Liu Y-L, Graves SE (2015) Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am 97:635–642
Vermue H, Luyckx T, Winnock de Grave P, Ryckaert A, Cools A-S, Himpe N, Victor J (2020) Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg Sports Traumatol Arthrosc 30(20):593–602
Yun AG, Qutami M, Pasko KBD (2021) Do bicortical diaphyseal array pins create the risk of periprosthetic fracture in robotic-assisted knee arthroplasties? Arthroplasty 3:25
Zaffagnini S, Di Paolo S, Meena A, Alesi D, Zinno R, Barone G, Pizza N, Bragonzoni L (2021) Causes of stiffness after total knee arthroplasty: a systematic review. Int Orthop 45:1983–1999
Zhang J, Ndou WS, Ng N, Gaston P, Simpson PM, Macpherson GJ, Patton JT, Clement ND (2021) Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06464-4
Funding
Open access funding provided by UMIT TIROL-Private Universität für Gesundheitswissenschaften und -technologie GmbH.
Author information
Authors and Affiliations
Contributions
Conceptualisation, CF, CN, AM and AE; methodology, AM, CN, AE and CF; data curation and synthesis, AM, CN and CF; writing—original draft preparation, AM, CN, AE and CF; writing—review and editing, AM, CN, AE and CF; supervision, CF; all authors interpreted the data, critically reviewed the work, made important contributions to the manuscript with their suggestions for improvement, approved the published version and agreed to be responsible for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest related to this study.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nogalo, C., Meena, A., Abermann, E. et al. Complications and downsides of the robotic total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 31, 736–750 (2023). https://doi.org/10.1007/s00167-022-07031-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07031-1